The Department of Chemistry has a longstanding record of excellence in chemical research, resulting in its reputation as one of the premiere institutions in the nation for the practice of research in the chemical sciences. Our faculty, postdoctoral fellows and graduate students together conduct innovative, ground-breaking research in all areas of modern chemistry — analytical, inorganic, organic, physical, materials, chemical biology, and chemical physics.
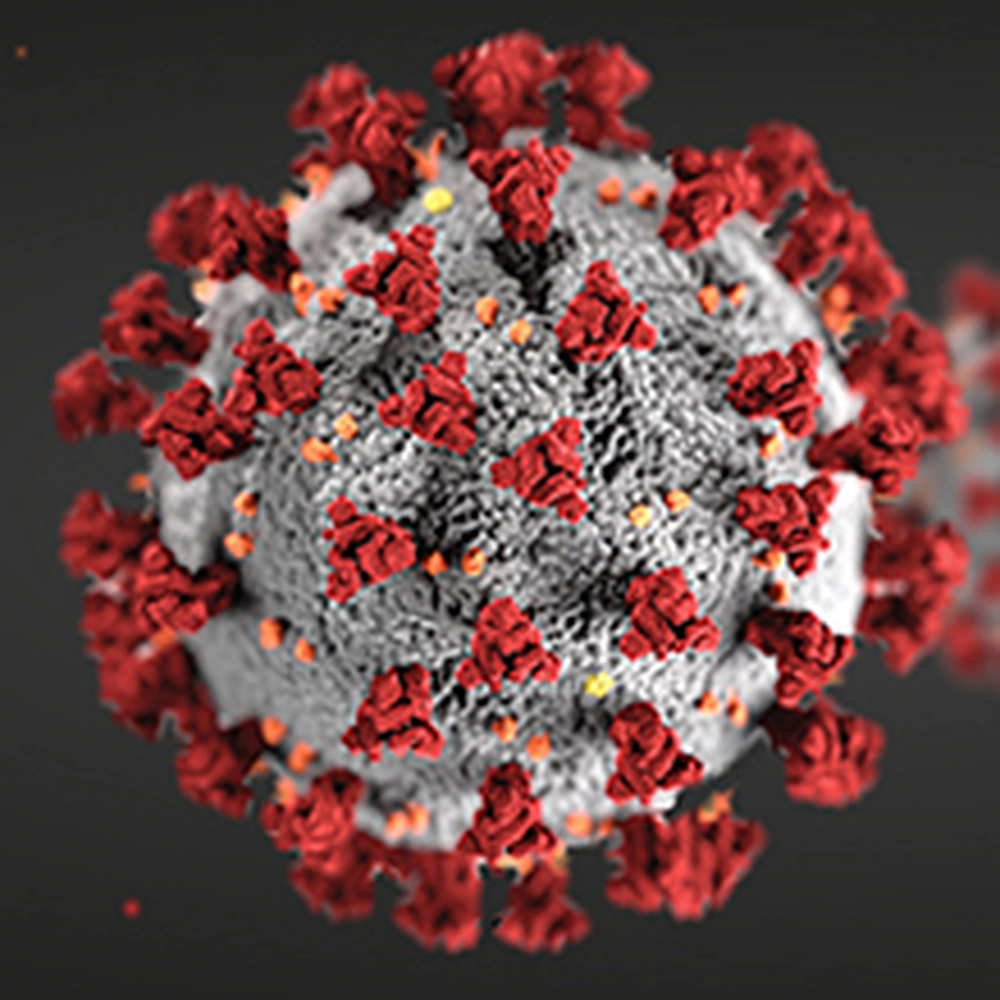
Read about some of the Department's most recent research projects and read more on this page about the various ongoing projects related to SARS-CoV-2.
From better COVID-19 testing to stopping the virus altogether
Researchers in the Department of Chemistry have been applying their expertise to this healthcare crisis in a variety of ways, from developing more accurate widely-deployable testing methods to better detect COVID-19 to stopping the virus, and future coronavirus pathogens, altogether.
Early in the pandemic, efforts focused on immediate needs of frontline healthcare workers. Professor Martin Burke was involved with a team of engineers, physicians, researchers and designers from the university and from Carle Health who developed and launched production of a face shield for health professionals responding to COVID-19 cases. Throughout the pandemic, Burke and chemistry professor Paul Hergenrother have been involved in the SHIELD initiative, leading the deployment on campus of a rapid COVID-19 virus and virus-antibody testing system. Since summer 2020, the university has been performing this rapid, saliva-based COVID-19 test on campus, testing thousands of students, faculty and staff each week. The direct saliva testing method developed by the team addressed bottlenecks of time, cost and supplies, and its unique features enable fast and frequent testing on a large scale. It is now being made available outside the U of I system. Hergenrother explains the development of the saliva-based test: "COV-Course: A Multidisciplinary Approach to Understanding the Pandemic."
The aggressive, innovative testing at the university has garnered national attention and an award, and UIUC received the inaugural Research Response to Community Crisis Award from the Association of Public and Land-grant Universities for its COVID-19 testing program. In August 2021, University of Illinois President Tim Killeen honored 28 people with the Presidential Medallion, including Burke, Hergenrother and chemistry lab technician Kelsie Green, for their leadership in the UI system’s COVID-19 response. The medallion is the highest honor that the system president can bestow.
Research projects:

Angad Mehta: The search for universal coronavirus vaccines
In addition to the current COVID-19 strategies of increasing testing capabilities and practicing social distancing, it has become imperative to develop therapeutic strategies as well, like drugs that can help treat patients and vaccines that can ultimately prevent the disease caused by the virus.
The universal vaccine platforms that Professor Angad Mehta envisions could be fundamentally important and groundbreaking and positively impact both short-term and long-term vaccine strategies that are imperative in tackling this global challenge. To carry out this research, he has received a grant from the National Science Foundation, specifically a RAPID grant for COVID-19-related projects.
Several therapeutic options, including various vaccine candidates are in clinical trials now, but as Mehta explains, the constant and sudden emergence of new coronavirus derived pathogens, including the SARS-CoV-2, accentuates the need to develop coronavirus vaccine platforms that can be broadly applied to all coronaviruses and then rapidly and rationally modified based on any emerging coronavirus derived pathogens.
This is especially important, he explained, considering continuing waves of infections.
For those reasons, the central goal of his study is to develop universal platforms to design vaccine candidates for coronaviruses, including SARS-CoV-2, that are based off altering the molecular details of coronavirus genome replication, transcription and translation.
Like the small molecule drug strategies which have shown very promising results by targeting the way in which these viruses replicate, Mehta envisions developing a universal live attenuated SARS-CoV-2 vaccine platform by engineering highly conserved coronavirus replication and transcription mechanisms.
Because these mechanisms are highly conserved, or identical, his platform will have the potential to be a universal and modular platform to engineer coronavirus vaccine candidates.
“So, we are targeting mechanisms that are identical in all known coronavirus pathogens; this makes it possible for our platform to be potentially modular and universal,” he said. “This is a bit different from current vaccine strategies that target proteins on the surface of the virus, where mutations have now been detected in these proteins.”
Furthermore, Mehta explained, several differences have also been observed in these proteins when compared to other coronavirus pathogens, including the SARS-CoV pathogen from the early 2000s.
“Therefore developing universal vaccine platforms might have implications on both short-term and long-term vaccine strategies to tackle this global challenge of developing vaccines for COVID-19 as well as future coronavirus pathogens,” he said.
Wilfred van der Donk: Trying to stop the virus from entering human cells
If Professor Wilfred van der Donk can stop the virus from entering human cells, it would prevent the COVID-19 virus infection altogether.
Van der Donk, the Richard E. Heckert Endowed Chair in Chemistry, explained how the SARS-CoV-2 virus that causes COVID-19 enters human cells by recognition of a surface receptor called the human acetyl choline esterase 2 (ACE2).
“The SARS-CoV-2 spike protein, so called because it is the protein that is responsible for the ‘spiky’ protrusions that are shown in artistic renditions of the virus, binds to ACE2 in the first step of entry into human cells,” he said. “If this entry can be stopped, virus infection will be prevented.
The molecular structure of the spike protein bound to ACE2 is known, van der Donk said, and the laboratory of Erik Procko in the Department of Biochemistry at Illinois has studied this interaction.
Compounds that mimic the part of the ACE2 protein where the spike protein binds could in principle work as decoys that bind to the virus and prevent it from interacting with ACE2, and that approach to fighting COVID-19 is what the van der Donk and Procko laboratories are exploring together.
“We use so-called lanthipeptides that resemble the part of ACE2 where the spike protein binds,” van der Donk explained. “Lanthipeptides are very stable compounds made in nature and are already used in the food industry to kill food-borne pathogens.”
Professor Xing Wang: Better, faster COVID-19 detection methods
With the support of a National Science Foundation RAPID grant, chemistry professor Xing Wang is working along with Brian Cunningham, a professor in Electrical and Computer Engineering at Illinois, to develop a new sensing paradigm for virus diagnostics that does not require the chemical enzymatic amplification of nucleic acids. This would eliminate the need for temperature control, thermal cycles, viral lysis, nucleic acid purification, or fluorescent dyes in virus testing. Their entire virus sensing process, explained below, is estimated to provide COVID-19 test results in less than 15 minutes.
According to Wang, their COVID-19 detection strategy combines two novel technologies recently developed in the labs of Wang and Cunningham.
First, they are using a designer DNA nanostructure-based technology developed in the Wang group, called Pattern-recognition Enabled Sensing and Therapeutics (PEST) to synthesize a customized DNA “virus net” that can recognize and capture intact SARS-CoV-2 virus particles with high binding avidity and specificity.
Second, the researchers then immobilize “virus net” on a photonic crystal biosensor surface to selectively attach the virus to the biosensor surface. The captured SARS-CoV-2 virions from patient samples are “imaged” by a new form of biosensor microscopy, developed in the Cunningham group, and called Photonic Resonator Interference Scattering Microscopy (PRISM), which allows users to detect and digitally count virus particles, protein molecules, and a variety of nanoparticles in real time without the use of additional labels or stains.
Burke and Hergenrother: SHIELD initiative
Burke is leading the SHIELD initiative that has strategically deployed rapid and scalable COVID-19 testing to detect the virus and virus antibodies by testing thousands of students, faculty and staff on campus each week with frontier modeling and contact tracing efforts. It's all been part of a broad integrated effort to reopen the university campus as safely as possible. The program centers on a three-part strategy dubbed Target, TEST, and Tell.
Burke is joined in this effort by a large number of partners from across campus, including chemistry Professor Paul Hergenrother, who developed the saliva-based COVID-19 test that has been key in the university campus re-opening and has gained national attention for its innovation.
A COVID-19 testing facility was created as a new arm of the Veterinary Diagnostic Lab on campus, which already has experience testing for COVID-19 in animals, and it combined efforts with other university entities, including the National Center for Supercomputing Applications and the new RokWire digital society, an interdisciplinary team of computer scientists and other experts on campus.
Burke said the considerable strengths of the NCSA, the new ROKWire digital society, and an intensive community engagement effort will be collectively interfaced with the data generated from this new lab to mitigate the risk that COVID-19 poses to the university community.
- How UIUC researchers fought the clock to develop the COVID-19 test that schools are using this fall.
- Group of 28 honored with Presidential Medallion for COVID-19 response efforts.
- Some College of Liberal Arts and Sciences alumni were also among the 28 medallion recipients.
- How the quick and inexpensive saliva screening is raising hopes for a less disruptive school year.
- The New York Times features the university's response to the pandemic.
- Watch a series of videos that chronicles the work of the SHIELD team: COVID-19 - YouTube.
Other COVID-19 efforts:
Burke and Doug Mitchell: Donation of testing components
Two initiatives took shape on campus to provide COVID-19 testing supplies that are in drastically short supply: one was focused on creating liquids necessary to conduct COVID-19 testing and the other was focused on the creation of nasopharyngeal swabs.
Chemistry’s Martin Burke and Doug Mitchell, Alumni Research Scholar Professor of Chemistry, collaborated with Microbiology’s Chris Brooke to mass produce liquids necessary for COVID-19 testing, including buffered saline and viral transfer media (VTM), an essential mix of buffers, nutrients, and antimicrobials that’s in short supply.
VTM is used to preserve test samples from patients until testing occurs. As faculty with appointments in the Carl R. Woese Institute for Genomic Biology, they were granted laboratory space in the institute to begin producing VTM using base materials from their own research supplies. A pair of laboratory technicians from Burke’s laboratory, Justin Lange and Akanksh Shetty, stepped forward to help, and soon the team was mass producing VTM. That caught the attention of state officials, who asked them to produce enough VTM for 10,000 tests per week. The VTM will be sent to a state laboratory in Springfield, with Illinois Emergency Management Agency reimbursing the university for the direct cost of the product.
As the agreement with the state of Illinois took shape, the Carl R. Woese Institute for Genomic Biology made available six more laboratory spaces, in addition to the one already being used, to scale up VTM production. More than 150,000 tubes of viral transfer media have been delivered to date, which has helped Illinois increase its testing capacity state wide.
“It has been deeply gratifying to see how faculty, staff, and students have stepped up to make it possible for the institute to contribute to this critical effort, from sourcing scarce materials, to facilitating deliveries, to organizing, training, and supervising staff, to actually preparing the VTM,” said Gene Robinson, Swanlund Chair of Entomology and director of the Carl R. Woese Institute for Genomic Biology. “This has been an inspirational team effort fueled by altruism.”
Mitchell said it hasn’t been easy to essentially turn an academic environment into a factory to fight COVID-19, but he is strongly motivated.
“Healthcare workers are those on the front lines of dealing with this disease; however, there is essentially no testing being done on those individuals who are exposed every day to patients with COVID-19,” he said. “How many people have been infected in hospitals and in the community through asymptomatic transmission of the virus? Without widespread testing, we will never know. The amount of testing that has been done thus far is a very far cry from what needs to be performed.”
Brooke said that it’s been stressful to get the testing up and running, but that he feels some satisfaction for making a difference.
“What we’re doing is small,” he added, “compared to the health workers who are actually serving patients on the front lines.”
This collaborative effort produced enough materials for nearly 200,000 coronavirus tests across the state.

Jeffrey Moore: Mass production of swabs to collect test samples
Early in the onset of the pandemic, a campus team focused on the mass production of nasopharyngeal swabs, which were in short supply and needed for collection of test samples from patients’ noses. In collaboration with Carle diagnostic labs, the team reverse-engineered a commercial swab to design and test their own.
The team, which included Mitchell, Jeffrey Moore, a Stanley O. Ikenberry Chair and professor of chemistry and materials science and engineering, and director of the Beckman Institute for Advanced Science & Technology, and Nancy Sottos, a Swanlund Chair and head of the Department of Materials Science and Engineering, developed a method to create enough swabs that, if validated, could meet a portion of the need in the state of Illinois.
The team also included Martin Gruebele, James R. Eiszner Endowed Chair in Chemistry and head of the Department of Chemistry, providing oversight as the plan required using glassware ovens found in organic chemistry labs in Roger Adams Lab to create the swabs. Mitchell described the process as converting a precursor rod into a viable swab using a hot draw. The key, he said, is to stretch the material in a way that retains rigidity in the handle while allowing for flexibility in the portion that enters the patient’s nose. The effort helped to produce up to 300,000 swabs to help deal with shortages.
“We came to the lab to reverse engineer the nasopharyngeal swab with a safe, inexpensive, rapid, scalable method from common laboratory supplies and equipment,” Moore said. “When our initial idea hit a snag, the graduate students put their ingenuity to work and improvised a brilliant solution that checked all the boxes.”