By Samantha Jones Toal
It has long been hypothesized that dietary habits can precede and even exacerbate the development of cancer.
Researchers at the Beckman Institute for Advanced Science and Technology proved that a direct link exists between the amount of fat included in one’s diet and bodily levels of nitric oxide, a naturally occurring signaling molecule that is related to inflammation and cancer development.
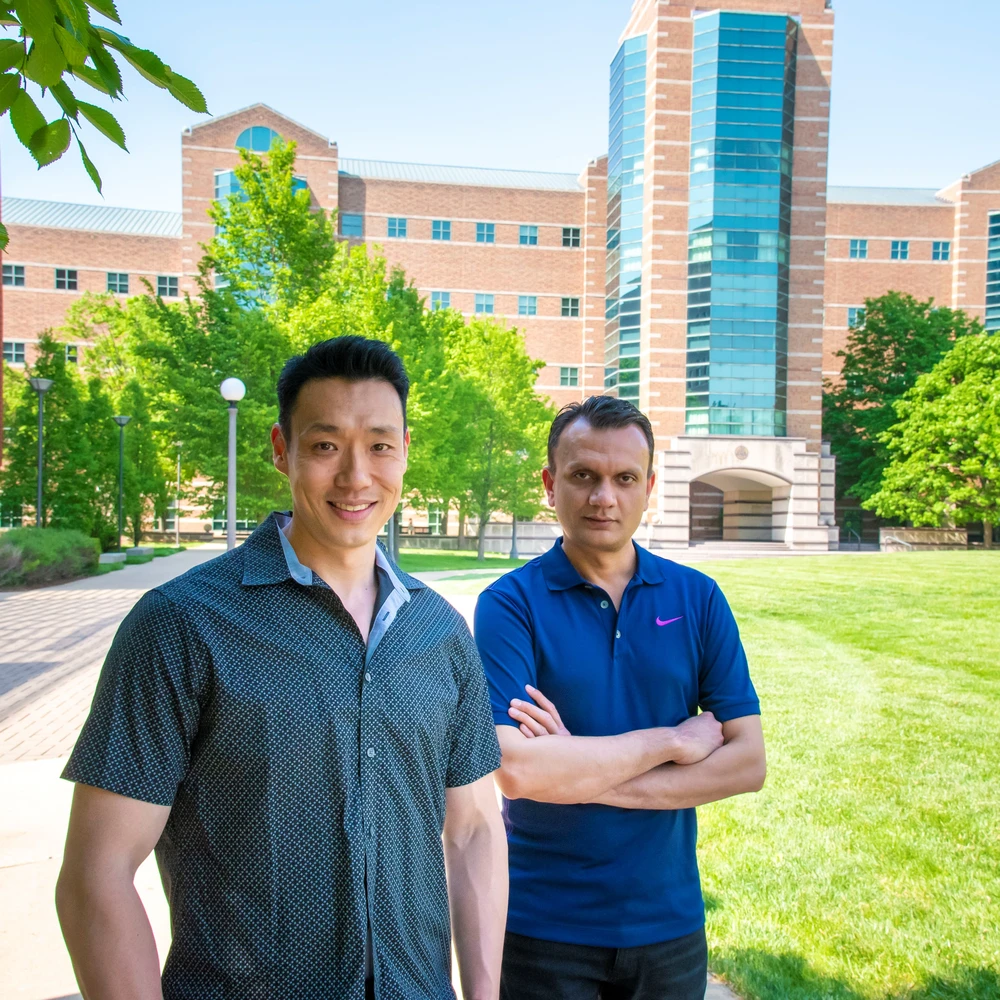
“We are trying to understand how subtle changes in the tumor microenvironment affect cancer progression at the molecular level. Cancer is a very complicated disease,” said Anuj Yadav, a senior research associate and the study's lead coauthor.
Yadav explained that cancer isn’t just about few tumor cells, but rather the entire microenvironment — or ecosystem — of the tumor supporting the cells.
“Inflammation can play a significant role in this environment. Certain inflammatory response comes from highly processed foods, which are high in calories and high in fat. We wanted to understand the links between food, inflammation, and tumors at a molecular level, so we had to develop advanced probes to be able to visualize these changes,” he said.
Yadav and coauthors are familiar with existing research linking increased nitric oxide levels to inflammation, and inflammation to cancer. Proving the connection between high-fat diets and nitric oxide levels on a molecular level required developing a highly sensitive molecular probe capable of deep-tissue imaging.
A molecular probe is a group of atoms or molecules used to study the properties of adjacent molecules by gauging the interactions between the probe and the structures of interest. But they are not one-size-fits-all. Each probe must be tailored to the conditions of its experiment.
“Our group specializes in making designer molecules, which allows us to look at molecular features that are invisible to the naked eye,” said Jefferson Chan, an associate professor of chemistry at the University of Illinois Urbana-Champaign and the study's principal investigator. “We design these custom-made molecules to discover things that weren’t previously known.”
The success of the study, which appeared in ACS Central Science in March, largely depended on the molecular probe designed by the team. Labeled BL660-NO, this probe is the first of its kind to be used in bioluminescence imaging of nitric oxide in cancer.
The researchers used the probe to design a diet study in mice, comparing the tumorigenicity of the breast-cancer-carrying mice on a high-fat diet (60% of calories coming from fat) with mice on a low-fat diet (10% of calories coming from fat) by measuring the nitric oxide levels in both groups.
“As a result of the high-fat diet, we saw an increase in nitric oxide in the tumor microenvironment,” said Michael Lee, a student researcher in the Chan lab and a lead coauthor on this study. “The implication of this is that the tumor microenvironment is a very complex system, and we really need to understand it to understand how cancer progression works. A lot of factors can go into this from diet to exercise — external factors that we don’t really take into account that we should when we consider cancer treatments.”
The authors emphasized the importance of proving a direct link between a high-fat diet, nitric oxide levels, and cancer development. With this association now known, new implications exist for cancer diagnosis and treatment.
“Without this technology, you wouldn’t see this missing molecular link," said Chan, who is also a faculty researcher at the Beckman Institute. “Now that we know that this is happening, how do we prevent it, and how do we improve the situation?”
This research in the news:
Editor's notes:
The paper “Activity-based NIR bioluminescence probe enables discovery of diet-induced modulation of the tumor microenvironment via nitric oxide” is accessible at: https://pubs.acs.org/doi/10.1021/acscentsci.1c00317?ref=pdf
For full author information, please consult the publication.
This research is supported by the National Institutes of Health.
The authors declare no competing financial interest.
Media contact: Jenna Kurtzweil, kurtzwe2@illinois.edu